OliClinomel
A three-chamber bag (3CB) formulated to meet the protein and energy needs of patients on parenteral nutrition (PN) and containing an olive oil-based lipid emulsion that may preserve immune function.4-7

Lipids are an essential component of parenteral nutrition (PN) therapy, but some lipid emulsions, based solely on soybean oil, should be limited due to their proinflammatory effects.1,2 OliClinomel contains ClinOleic, an olive oil-based lipid emulsion that has been associated with fewer infections and may preserve immune function.3-7 The OliClinomel portfolio offers a range of formulations suitable for both central and peripheral administration, all designed to meet patients’ individual protein and energy needs.3

OliClinomel contains ClinOleic, Baxter’s olive oil-based lipid emulsion
OliClinomel contains amino acids, lipids, and glucose. OliClinomel’s olive oil-based lipid emulsion is rich in omega-9 fatty acids and is associated with fewer infections and may preserve immune function.3-7

OliClinomel
Download the Baxter Parenteral Nutrition Compatibility Guide for compatibility and stability information.
Learn more about Clinical Nutrition

Related Products
Important safety information
This abbreviated summary of product characteristics (SPC) is intended for international use. Please note that it may differ from the licensed SPC in the country where you are practicing.Therefore, please always consult your country-specific SPC or package leaflet.
OLICLINOMEL
Emulsion for infusion.
Qualitative composition
This medicinal product is presented in the form of a 3-compartment bag. (Lipid emulsion compartment, amino acid compartment and glucose solution compartment)
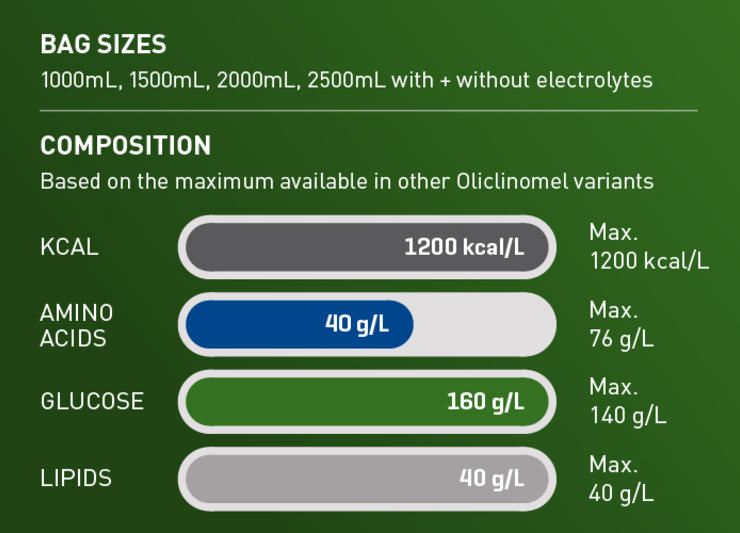
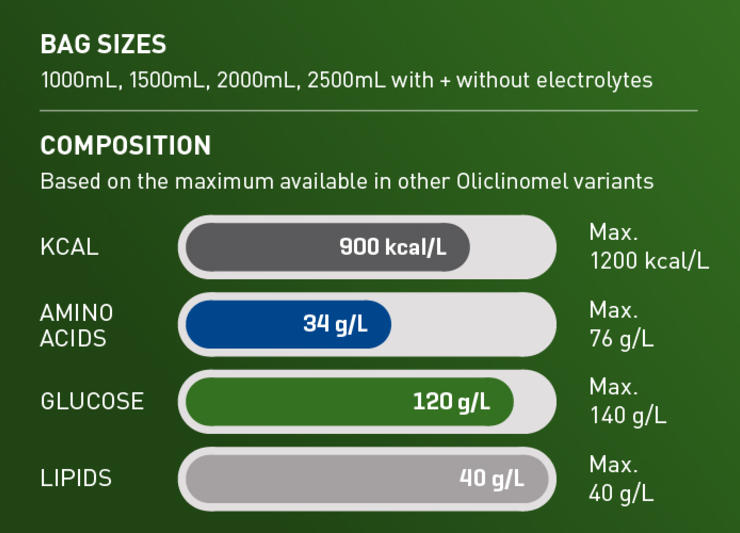
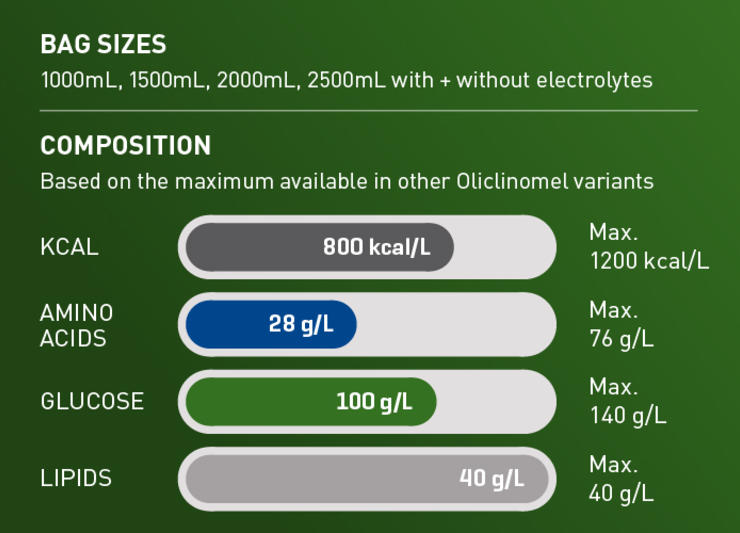
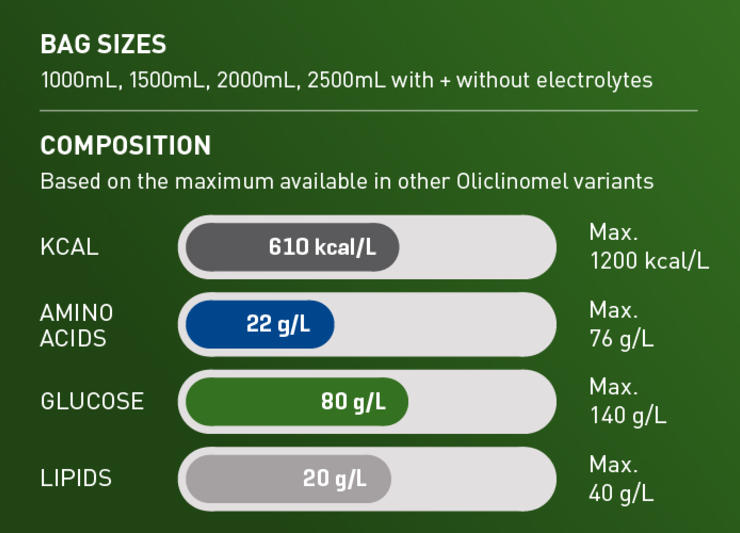
Oliclinomel exist in 8 different formula:
• N4-550 and N4-550E (with electrolytes): 1000ml contains 20g lipids, 22g amino acids and 80g glucose
• N5-800 and N5-800E (with electrolytes): 1000ml contains 40g lipids, 28g amino acids and 100g glucose
• N6-900 and N6-900E (with electrolytes): 1000ml contains 40g lipids, 34g amino acids and 120g glucose
• N7-1000 and N7-1000E (with electrolytes): 1000ml contains 40g lipids, 40g amino acids and 160g glucose
For each formula, there are four presentations: 1000ml, 1500ml, 2000ml and 2500ml
Active substances
Refined olive oil + refined soya oil*
Alanine, Arginine, Glycine, Histidine, Isoleucine, Leucine, Lysine (As lysine hydrochloride), Methionine, Phenylalanine, Proline, Serine, Threonine, Tryptophan, Tyrosine, Valine, Anhydrous glucose (As glucose monohydrate)
* Mixture of refined olive oil (approximately 80%) and refined soya oil (approximately 20%)
For the Oliclinomel formula with electrolytes, following substances are also present: Sodium Acetate 3H2O, Sodium glycerophosphate 5H2O, Potassium chloride, Magnesium chloride 6H2O, Calcium chloride 2H2O
Therapeutic indications
Parenteral nutrition for adults and children above 2 years of age when oral or enteral nutrition is impossible, insufficient or contraindicated.
Posology The dosage will depend on the patient’s energy expenditure, clinical status, body weight, and the ability to metabolize the constituents of OLICLINOMEL , as well as additional energy or proteins provided orally/enterally; therefore, the bag size should be chosen accordingly.The administration may be continued for as long as is required by the patient’s clinical conditions. Please check full SPC for more information about posology.
The maximum daily dose should not be exceeded in adult and paediatric patients.
Method of administration
For Oliclinomel N4-550 and N4-550E: By intravenous administration through a central or peripheral vein
For Oliclinomel N5-800, N5-800E, N6-900, N6-900E, N7-1000 and N7-1000E: By intravenous administration through a central vein
The recommended duration of the parenteral nutrition infusion is between 12 and 24 hours.
Contraindications
Use of OLICLINOMEL is contraindicated in the following situations:
- in premature neonates, infants and children less than 2 years old, as the calorie-nitrogen ratio and energy supply are inappropriate.
- known hypersensitivity to egg or soya proteins or to any other ingredient.
— congenital abnormalities of amino acid metabolism.
— severe hyperlipidaemia.
- Severe hyperglycemia.
-[For Oliclinomel formulations with electrolytes: Pathologically-elevated plasma concentration of sodium, potassium, magnesium, calcium, and/or phosphorus]
Special warnings and precautions for use
[For all Oliclinomel formulations except N4-550, and N4-550E: Do not administer through a peripheral vein]
An excessively fast administration of total parenteral nutrition (TPN) solutions, including OLICLINOMEL, may result in severe or fatal consequences.
The infusion must be stopped immediately if any signs or symptoms of an allergic reaction (such as sweating, fever, chills, headache, skin rashes, dyspnoea or bronchospasm) develop. This medicinal product contains soybean oil and egg phosphatide. Soybean and egg proteins may cause hypersensitivity reactions. Cross-allergic reactions between soybean and peanut proteins have been observed.
Hypersensitivity reactions in patients with allergy to corn or corn products.
Specific clinical monitoring is required when an intravenous infusion is started.
Severe water and electrolyte equilibration disorders, severe fluid overload states, and severe metabolic disorders must be corrected before starting the infusion.
For Oliclinomel formulations with electrolytes: Ceftriaxone must not be mixed or administered simultaneously with any calcium-containing IV solutions even via different infusion lines or different infusion sites. Cefriaxone and calcium-containing solutions may be administered sequentially one after another if infusion lines at different sites are used or if the infusion lines are replaced or thoroughly flushed between infusions with physiological salt solution to avoid precipitation
Pulmonary vascular precipitates causing pulmonary vascular embolism and respiratory distress have been reported in patients receiving parenteral nutrition. In some cases, fatal outcomes have occurred. Excessive addition of calcium and phosphate increases the risk of formation of calcium phosphate precipitates.
[For OLICLINOMEL N4-550, N5-800, N6-900 and N7-1000 formulations:] Precipitates of various natures have been reported even in the absence of phosphate salt in the solution.
Suspected precipitate formation in the blood stream has also been reported.
In addition to inspection of the solution, the infusion set and catheter should also periodically be checked for precipitates.
If signs of respiratory distress occur, the infusion should be stopped and medical evaluation initiated.
Do not add other medicinal products or substances to any components of the bag or to the reconstituted emulsion without first confirming their compatibility and the stability of the resulting preparation (in particular, the stability of the lipid emulsion). Formation of precipitates or destabilization of the lipid emulsion could result in vascular occlusion
Vascular-access infection and sepsis are complications that may occur in patients receiving parenteral nutrition, particularly in case of poor maintenance of catheters, immunosuppressive effects of illness or drugs. Careful monitoring of signs, symptoms, and laboratory tests results for fever/chills, leukocytosis, technical complications with the access device, and hyperglycaemia can help recognize early infections. Patients who require parenteral nutrition are often predisposed to infectious complications due to malnutrition and/or their underlying disease state.
Monitor water and electrolyte balance, serum osmolarity, serum triglycerides, acid-base balance, blood glucose, liver and kidney function tests, coagulation tests and blood count, including platelets throughout treatment.
Metabolic complications may occur if the nutrient intake is not adapted to the patient’s requirements, or the metabolic capacity of any given dietary component is not accurately assessed. Serum triglyceride concentrations and the ability of the body to remove lipids must be checked regularly.
Serum triglyceride concentrations must not exceed 3 mmol/l during the infusion. These concentrations should not be determined before a minimum of a 3-hour period of continuous infusion.
If a lipid metabolism abnormality is suspected, it is recommended that tests be performed daily by measuring serum triglycerides after a period of 5 to 6 hours without administering lipids. In adults, the serum must be clear in less than 6 hours after stopping the infusion containing the lipid emulsion. The next infusion should only be administered when the serum triglyceride concentrations have returned to normal values.
Fat overload syndrome has been reported with the administration of OLICLINOMEL and similar products.
In the event of hyperglycaemia, the infusion rate of OLICLINOMEL must be adjusted and/or insulin administered.
While OLICLINOMEL N4-550, N4-550E may be administered through a peripheral vein, thrombophlebitis may develop. The catheter insertion site must be monitored daily for local signs of thrombophlebitis.
When making additions, the final osmolarity of the mixture must be measured before administration.
Although there is a natural content of trace elements and vitamins in the product, the levels are insufficient to meet body requirements and these should be added to prevent deficiencies from developing.
Caution should be exercised in administering OLICLINOMEL to patients with increased osmolarity, adrenal insufficiency, heart failure or pulmonary dysfunction.
Refeeding severely undernourished patients may result in the refeeding syndrome that is characterized by the shift of potassium, phosphorus, and magnesium intracellularly as the patient becomes anabolic. Thiamine deficiency and fluid retention may also develop. Careful monitoring and slowly increasing nutrient intakes while avoiding overfeeding can prevent these complications. This syndrome has been reported with similar products.
Do not connect bags in series in order to avoid the possibility of air embolism due to residual air contained in the primary bag.
Hepatic Insufficiency
Use with caution in patients with hepatic insufficiency because of the risk of developing or worsening neurological disorders associated with hyperammonaemia.
Renal Insufficiency
Use with caution in patients with renal insufficiency, particularly if hyperkalaemia is present, because of the risk of developing or worsening metabolic acidosis and hyperazotemia if extra-renal waste removal is not being performed.
Hematologic
Use with caution in patients with coagulation disorders and anaemia.
Endocrine and Metabolism
Use with caution in patients with:
• Metabolic acidosis. Administration of carbohydrates is not recommended in the presence of lactic acidosis. Regular clinical and laboratory tests are required.
• Diabetes mellitus. Monitor glucose concentrations, glucosuria, ketonuria and, where applicable adjust insulin dosages.
• Hyperlipidaemia due to the presence of lipids in the emulsion for infusion. Regular clinical and laboratory tests are required.
• Amino acid metabolism disorders
Extravasation
Catheter site should be monitored regularly to identify signs of extravasation
Interactions with other medicinal products and other forms of interactions
For Oliclinomel formulations with electrolytes: Precipitation of ceftriaxone-calcium can occur when ceftriaxone is mixed with calcium-containing solutions in the same intravenous administration line This emulsion for infusion must not be administered simultaneously with blood through the same infusion tubing because of the possibility of pseudoagglutination.
OLICLINOMEL contains vitamin K, naturally present in lipid emulsions. The amount of Vitamin K in recommended doses of OLICLINOMEL are not expected to influence effects of coumarin derivatives.
This emulsion for infusion must not be administered simultaneously with blood through the same infusion tubing because of the possibility of pseudoagglutination.
Oliclinomel with electrolytes: Due to the potassium content of OLICLINOMEL, special care should be taken in patients treated with potassium sparing diuretics (e.g., amiloride, spironolactone, triamterene), angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists or the immunosuppressants tacrolimus and cyclosporine in view of the risk of hyperkalemia.
Fertility, pregnancy and lactation
There are not at present sufficient relevant clinical findings to assess the tolerability of the ingredients in OLICLINOMEL in women who are pregnant or breast-feeding.
Shelf life
2 years if the overwrap is not damaged.
It is recommended that the product is used immediately after the non-permanent seals between the 3 compartments have been opened.
For the Quantitative Composition, Posology, incompatibilities and undesirable effects, please refer to the full SPC.
Medicinal products are subject to medical subscription.
Date of preparation: Jan 2019
This abbreviated summary of product characteristics (SPC) is intended for international use. Please note that it may differ from the licensed SPC in the country where you are practicing.
Therefore, please always consult your country-specific SPC or package leaflet.
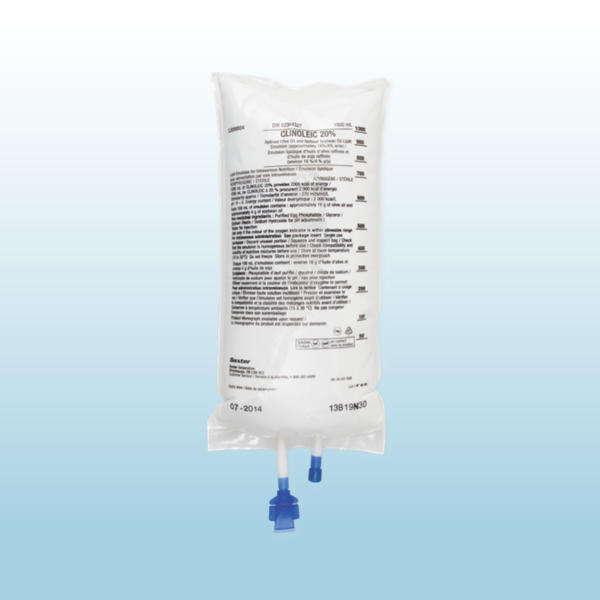
ClinOleic 20%:
Emulsion for infusion.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Per 100 ml: Refined olive oil and refined soya bean oil* 20.00 g corresponding to a content of essential fatty acids 4.00 g. Energy content 2000 kcal/l (8.36 MJ/l).Lipid content (olive and soya bean oil) 200 g/l.Osmolarity 270 mOsm/l.pH 6 -8 Density 0.986.Phospholipids provide 47 milligrams or 1.5 mmol of phosphorus per 100 ml.
*Mixture of refined olive oil (approximately 80%) and refined soya bean oil (approximately 20%).
CLINICAL PARTICULARS
Therapeutic indications:
Indicated as a source of lipids for patients requiring parenteral nutrition, when oral or enteral nutrition is impossible, insufficient or contraindicated.
Posology and method of administration:
Clinoleic 20% contains 200 mg/ml of lipids.
The posology depends on energy expenditure, the patient’s clinical status, body weight, and ability to metabolize ClinOleic 20%, as well as additional energy given orally/enterally. Therefore, the dosage should be individualized and the bag size chosen accordingly.
Dosage:
In adults: The posology is 1 to a maximum of 2 g lipids/kg/day. The initial infusion rate must be slow and not exceed 0.1 g lipids or 0.5 ml (10 drops) per minute for 10 minutes then gradually increased until reaching the required rate after half an hour. Never exceed 0.15 g lipids/kg/hour (0.75 ml/kg/hour). Adults per kg of body weight: Usual lipid dosage: 1 to 2 g/kg/day. Infused volume of Clinoleic 20%:5 to 10 ml/kg/day. Adults for 70 kg: Usual lipid dosage: 70 to 140 g/day. Infused volume of Clinoleic 20%: 350 to 700 ml/day.
In children: Clinoleic 20% should be administered as a continuous 24h/day infusion. It is recommended not to exceed a daily dose of 3g-lipids/kg b.w. and an infusion rate of 0.15 g lipids/kg b.w./h. Daily dose should be increased gradually during the first week of administration.
In premature newborns and low birth weight infants: The use of Clinoleic 20% is restricted to premature infants of 28 weeks of gestational age or more. Clinoleic 20% should be administered as a continuous 24h/day infusion. The initial daily dose should be 0.5-1.0g lipids/kg b.w. The dose may be increased by 0.5-1.0g lipids/kg b.w. every 24 hours up to a daily dose of 2.0 g lipids/kg b.w. Usage in nutritive admixtures (with glucose and amino acids): “Breaking” or “oiling out” of the emulsion can be visibly identified by accumulation of yellowish droplets or particles in the admixture
Contraindications:
- hypersensitivity to the active substance or to any of the excipients (e.g.: egg or soybean protein)
- severe dyslipidemia and non corrected metabolism disorders including lactic acidosis and uncompensated diabetes
Special warnings and special precautions for use:
The infusion must be stopped immediately if any abnormal signs or symptoms of an allergic reaction (such as sweating, fever, shivering, headache, skin rashes or dyspnoea) develop. This medicinal product contains soya-bean oil and egg phospholipids. Soybean and egg proteins may cause hypersensitivity reactions. Cross-allergic reactions between soybean and peanut proteins have been observed.
During short-term or long-term intravenous nutrition, alkaline phosphatases and total bilirubin should be checked at regular intervals, depending on the health status of the patient. The blood sugar, serum triglycerides, the acid-base balance, electrolytes, serum osmolarity, kidney function, coagulation parameters and the blood count must be checked at regular intervals.
Parenteral nutrition should be used with caution in patients with pre-existing liver disease or liver insufficiency. Liver function parameters should be closely monitored in these patients.
Parenteral Associated Liver Diseases (PNALD) including cholestasis, hepatic staetosis, fibrosis and cirrhosis, possibly leading to hepatic failure, as well as cholecystitis and cholelithiasis are known to develop in some patients on parenteral nutrition. The etiology of these disorders in thought to be multifactorial and may differ between patients. Patients developing abnormal laboratory parameters or other signs of hepatobiliary disorders should be assessed early by a clinician knowledgeable in liver diseases in order to identify possible causative and contributory factors, and possible therapeutic and prophylactic interventions.
Clinoleic 20% should be administered with caution in case of neonatal hyperbilirubinemia (total serum bilirubin > 200 μmol/ l). Total bilirubin levels should be monitored closely. As other lipid emulsions, Clinoleic 20% should be used in extremely premature and/or very low birth-weight infant under the close supervision of a neonatologist. There is clinical experience for Clinoleic 20% infusion time, up to 7 days in neonates and up to 2 months in children. Light exposure of solutions for intravenous parenteral nutrition, especially after admixture with trace elements and/or vitamins, may have adverse effects on clinical outcome in neonates, due to generation of peroxides and other degradation products. When used in neonates and children below 2 years, Clinoleic should be protected from ambient light until administration is completed
Interactions with other medicaments and other forms of interaction: Complete information about incompatibilities is not available. ClinOleic 20% contains vitamin K, naturally present in lipid emulsions. The amount of Vitamin K in recommended doses of ClinOleic 20%, are not expected to influence effects of coumarin derivatives.
The lipids contained in this emulsion may interfere with the results of certain laboratory tests if the blood sample is taken before the lipids are eliminated from the serum (these are generally eliminated after a period of 5 to 6 hours without receiving lipids). Refer to the laboratory testing system product information regarding potential assay interference associated with lipemic samples.
Pregnancy and lactation: The safety of administration of Clinoleic 20% during pregnancy and lactation has not been established. Therefore, Clinoleic 20% should not be used during pregnancy and lactation except after special consideration.
Undesirable effects:
Common: nausea vomiting, hyperglycaemia, mean arterial pressure decreased.
Uncommon: Dyspnea, Cholestasis, Blood bilirubin increased, Hepatic enzyme increased.
Overdose: A reduced ability to remove the lipids may result in a "fat overload syndrome" which may be caused by overdose, the effects of which are usually reversible after the lipid infusion is stopped.
PHARMACEUTICAL PARTICULARS:
List of excipients:
Egg phospholipids, glycerol, sodium oleate, sodium hydroxide, water for injections.
Incompatibilities:
Complete information about incompatibilities is not available. Never add medication or electrolytes directly to the lipid emulsion. If it is necessary to introduce additives, verify the compatibility and mix thoroughly before administration to the patient.
Shelf life:
18 months in plastic bag in its overwrap. When used in neonates and children below 2 years, the solution (in bags and administration sets) should be protected from light exposure until administration is completed.
Special precautions for storage:
Do not store above 25°C.Do not freeze. Keep the container in the outer carton.
Medicinal products subject to medical prescription.
Date of preparation: Mar 2020