Neonatology
Optimizing parenteral nutrition (PN) therapy in preterm infants and neonates through advanced solutions including industry-prepared licensed, ready-to-use three-chamber-bags
Adequate nutritional intake is essential for promoting growth and immunity as well as long-term metabolic, cognitive, and neurodevelopmental health. Most preterm infants, especially those born before 28 weeks of gestation, can face significant nutritional challenges in the early days and weeks of life.1 PN therapy is an essential part of neonatal care, and international guidelines strongly recommend that standard rather than individualized PN solutions are used in most newborn patients requiring PN therapy including premature infants with very low birthweight (VLBW).2 Baxter provides various standard PN solutions for newborns including the first and only licensed ready-to-use three-chamber-bag (3CB) solution specifically designed for neonatal patients.3,4
Neonatal growth is critical for positive outcomes
Worldwide, one in every ten babies is born preterm. This adds up to 15 million preterm babies every year.5 Preterm birth complications are the leading cause of death for children below 5 years of age.6 Approximately half of VLBW infants experience postnatal growth failure which can affect long-term psychomotor development.7,8 Moderate to late preterm infants are at an increased risk of delayed development in areas such as language, social emotional competencies, cognition, and motor skills.9
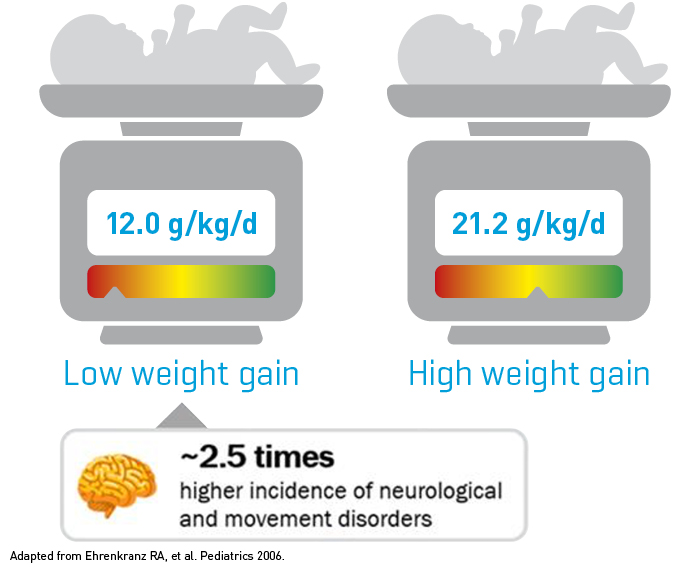
Growth velocity during early neonatal life exerts a significant effect on neurodevelopmental and growth outcomes as the child ages. An observational study showed that preterm infants with a low weight gain from birth to discharge had a 2.5 times higher incidence of neurological and movement disorders as compared to preterm infants with a high weight gain.10
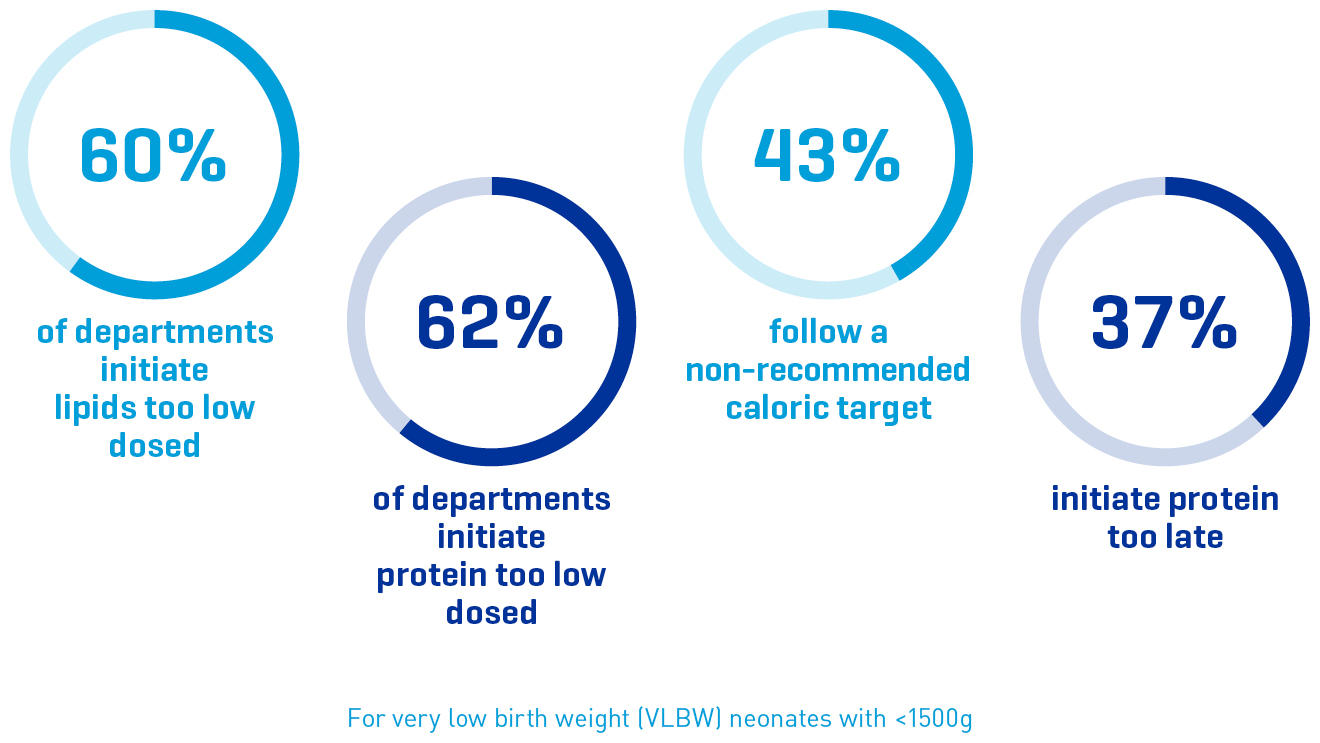
Parenteral nutrition in VLBW neonates is frequently too low dosed
The complexity of individualized compounded PN, with approximately 50 components being combined, presents ample opportunity for compounding errors and contamination.13
37%
error rate has been documented for manually compounded PN.14
22%
error rate has been documented for semi-automatically prepared PN.14