Clinimix
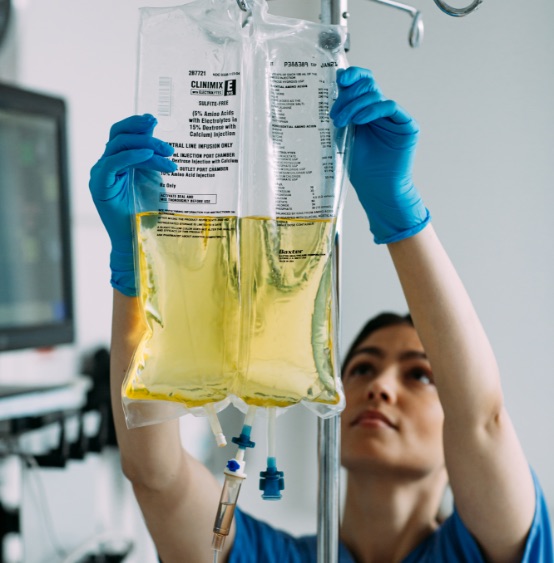
Portfolio of dual-chamber ready-to-use parenteral nutrition (PN) products designed to offer a range of amino acid and dextrose combinations while meeting the basic amino acid and energy needs of patients.

With over 25 years of experience, Clinimix dual-chamber bags enable clinicians to meet the protein and energy requirements of each patient, while at the same time offering the flexibility to add lipids as needed. The Clinimix portfolio offers a range of bag sizes with formulations suitable for central and peripheral administration.1
Clinimix
Download the Baxter Parenteral Nutrition Compatibility Guide for compatibility and stability information.
Learn more about Clinical Nutrition

Related Products
Important safety information
This abbreviated summary of product characteristics (SPC) is intended for international use. Please note that it may differ from the licensed SPC in the country where you are practicing.Therefore, please always consult your country-specific SPC or package leaflet.
NAMES OF THE MEDICINAL PRODUCT
CLINIMIX N9G20E, CLINIMIX N9G15E ,CLINIMIX N9G20E, CLINIMIX N12G20, CLINIMIX N12G20E, CLINIMIX N14G30, CLINIMIX N14G30E, CLINIMIX N17G35, CLINIMIX N17G35E, solution for infusion
QUALITATIVE COMPOSITION
CLINIMIX N9G20E, CLINIMIX N9G15E ,CLINIMIX N9G20E, CLINIMIX N12G20E, CLINIMIX N14G30E, CLINIMIX N17G35E, are packaged in a dual compartment plastic bag containing respectively an amino acid solution with electrolytes and a glucose solution with calcium.
CLINIMIX N12G20 ,CLINIMIX N14G30, CLINIMIX N17G35, are packaged in a dual compartment plastic bag containing respectively an amino acid solution without electrolytes and a glucose solution without calcium.
Please check full SPC for full Quanitative composition.
CLINICAL PARTICULARS
Therapeutic indications
Parenteral nutrition when oral or enteral alimentation is impossible, insufficient or contraindicated.
For patient undergoing long-term parenteral nutrition, the addition of a lipid emulsion to CLINIMIX in order to supply both calories and essential fatty acids is possible.
Contraindications
Known hypersensitivity to any of the active substances or excipients, or to the components of the container. • Amino acid metabolism disorders • Severe hyperglycaemia • Metabolic acidosis, hyperlactataemia • CLINIMIX containing electrolytes: should not be used in patients with hyperkalaemia, hypernatraemia and in patients with pathologically elevated plasma concentrations of magnesium, calcium and/or phosphorus. • As for other calcium-containing infusion solutions, concomitant treatment with ceftriaxone and CLINIMIX containing electrolytes is contraindicated in newborns (≤28 days of age), even if separate infusion lines are used (risk of fatal ceftriaxone calcium salt precipitation in the neonate’s bloodstream).
Undesirable effects
Potential undesirable effects may occur as a result of inappropriate use: for example, overdose or excessively fast infusion rate.
Post-marketing Adverse Reactions
The following adverse reactions have been reported with CLINIMIX formulations in the postmarketing experience, listed by MedDRA System Organ Class (SOC) and by Preferred Term
|
System Organ Class (SOC) |
Preferred MedDRA Term |
Frequencya |
|
Immune system disorders |
Hypersensitivity* |
Not known |
a: Frequency is defined as very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1000 to < 1/100): rare (≥ 1/10,000 to < 1/1000); very rare (< 1/10,000); and not known (cannot be estimated from the available data).
*Includes the following manifestations: Hypotension, Hypertension, Peripheral cyanosis, Tachycardia, Dyspnoea, Vomiting, Nausea, Urticaria, Rash, Pruritus, Erythema, Hyperhidrosis, Pyrexia, Chills
Class Reactions: Other adverse reactions reported with parenteral nutrition include: • Anaphylaxis • Pulmonary vascular precipitates • Hyperglycaemia; Hyperammonemia, Azotemia • Hepatic failure, Hepatic cirrhosis, Hepatic fibrosis, Cholestasis, Hepatic steatosis, Blood bilirubin increased, Hepatic enzyme increased • Cholecystitis, Cholelithiasis • Infusion site thrombophlebitis, Venous irritation (Infusion site phlebitis, Pain, Erythema, Warmth, Swelling, Induration).
Glucose intolerance is a common metabolic complication in severely stressed patients. With the infusion of the products, hyperglycaemia, glycosuria, and hyperosmolar syndrome may occur.
Precautions
Severe water and electrolyte equilibration disorders, severe fluid overload states, and severe
metabolic disorders should be corrected before starting the infusion.
Metabolic complications may occur if the nutrient intake is not adapted to the patient's requirements, or the metabolic capacity of any given dietary component is not accurately assessed. Adverse metabolic effects may arise from administration of inadequate or excessive nutrients or from inappropriate composition of an admixture for a particular patient's needs.
Frequent clinical evaluation and laboratory determinations are necessary for correct monitoring during administration. These should include ionogram and kidney and liver function tests.
The electrolyte requirements of patients receiving the solutions should be carefully determined and monitored especially for the electrolyte-free solutions. CLINIMIX without electrolytes should not be used in cases of hypokalaemia and hyponatremia.
Glucose intolerance is a common metabolic complication in severely stressed patients. With the infusion of the products, hyperglycaemia, glycosuria, and hyperosmolar syndrome may occur. Blood and urine glucose should be monitored on a routine basis and for diabetics insulin dosage should be adapted, if necessary.
Use with caution in patients with renal insufficiency, particularly if hyperkalaemia is present, because of the risk of developing or worsening metabolic acidosis and hyperazotemia if extra- renal waste removal is not being performed. Fluid and electrolyte status should be closely monitored in these patients. In case of severe kidney failure, specially formulated amino acid solutions should be preferred.
Caution should be exercised in administering CLINIMIX to patients with adrenal insufficiency.
Care should be taken to avoid circulatory overload particularly in patients with pulmonary oedema, cardiac insufficiency and/or failure. Fluid status should be closely monitored.
In patients with pre-existing liver disease or hepatic insufficiency, apart from routine liver function tests, possible symptoms of hyperammonaemia should be controlled.
Hepatobiliary disorders including cholestasis, hepatic steatosis, fibrosis and cirrhosis, possibly leading to hepatic failure, as well as cholecystitis and cholelithiasis are known to develop in some patients on parenteral nutrition. The aetiology of these disorders is thought to be multifactorial and may differ between patients. Patients developing abnormal laboratory parameters or other signs of hepatobiliary disorders should be assessed early by a clinician knowledgeable in liver diseases in order to identify possible causative and contributory factors, and possible therapeutic and prophylactic interventions.
Increase in blood ammonia levels and hyperammonemia may occur in patients receiving amino acid solutions. In some patients this may indicate the presence of a congenital disorder of amino acid metabolism (see section 4.3) or hepatic insufficiency.
Blood ammonia should be measured frequently in newborns and infants to detect hyperammonemia, which may indicate the presence of a congenital abnormality of amino acid metabolism.
Depending on extent and aetiology, hyperammonemia may require immediate intervention.
A too rapid infusion of amino acids may result in nausea, vomiting and chills. In such cases, discontinue the infusion immediately.
In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or drug therapy.
Paediatric population: This medicinal product is not recommended for preterm, and term neonates and for children below 2 years of age.See above regarding monitoring for hyperammonemia in patients below 2 years.
Light exposure of solutions for intravenous parenteral nutrition, especially after admixture with trace elements and/or vitamins, may have adverse effects on clinical outcome in neonates, due to generation of peroxides and other degradation products. When used in neonates and children below 2 years, Clinimix should be protected from ambient light until administration is completed
For the detailed composition, posology, Special warnings and precautions for use, interactions, pharmacological properties and pharmaceutical particulars, please refer to the full SPC. Medicinal products are subject to medical prescription
Revised Apr 2021